The Benefits of Clinical Pilates on Lower Back Pain
Lower back pain (LBP) is the leading cause of disability worldwide, affecting up to 80% of people at some point in their lives (Hartvigsen et al., 2018). In Australia, it is a primary driver of work absenteeism (Smith et al., 2021) and reduced quality of life (Alshehri et al., 2023). While most acute episodes resolve within six weeks with the right care, approximately 30% of patients will develop chronic symptoms without timely and appropriate intervention (Ferreira et al., 2023). Fortunately though, the vast majority of LBP is mechanical and highly responsive to targeted physiotherapy and structured exercise rehabilitation (Qaseem et al., 2020), with Clinical
Pilates emerging as an effective for of treatment during rehabilitation.
Why Mechanical Back Pain Persists


Mechanical LBP stems from altered movement, poor load management, and impaired muscular stability. Key contributors include:
- Poor lumbo-pelvic control and weakness of deep stabilisers (multifidus, transversus abdominis)
- Discogenic pain, degeneration, joint hypomobility and joint overload
- Movement imbalances and faulty motor patterns across the kinetic chain (e.g., weak glutes, tight hips, impaired knee or ankle function)
- Psychosocial factors like fear-avoidance and deconditioning, which can worsen outcomes (Borst et al., 2023)
Physiotherapy Assessment of Lower Back Pain
A thorough physiotherapy assessment is foundational to effective management of LBP. Our physiotherapists conduct detailed evaluations of posture, movement patterns, core muscle control, and functional limitations, identifying mechanical contributors such as the above mentioned lumbo-pelvic stability issues, muscle imbalances, joint hypomobility or movement dysfunction (Alqarni et al., 2022). This includes screening for red flags requiring urgent medical referral. This individualised assessment allows our clinicians to tailor treatment plans to the patient’s specific history, lifestyle and goals, leading to improved outcomes and prevention of chronicity (Borst et al., 2023).
Guidelines advise against routine scans for non-specific LBP under 12 weeks without red flags, due to its minimal impact on management (Chou et al., 2020), however clinical reasoning is essential as there are times with imaging is imperative.
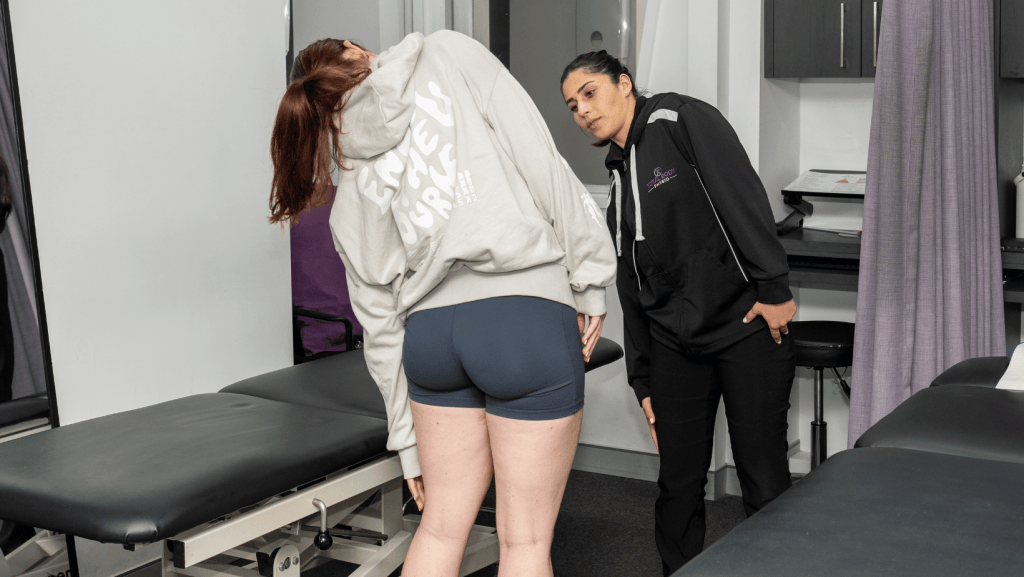
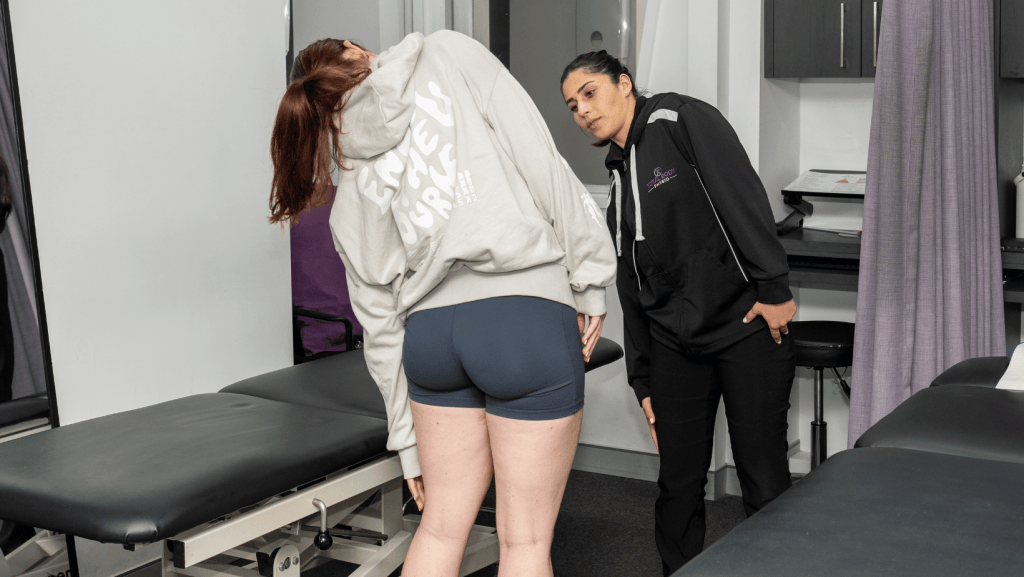
Physiotherapy Treatment
Evidence supports structured physiotherapy treatment as a cornerstone in managing both acute and chronic LBP (Zadro et al., 2023). In our clinic, treatment often involves manual therapy to improve joint hypomobility and pain, patient education on load, posture and ergonomics, and supervised exercises aimed at restoring flexibility, motor control, core strength and global strength (Narenthiran et al., 2025). Clinical Pilates is a highly effective physio-led modality that integrates these elements to address the root causes of pain and dysfunction (O’Neil et al., 2020). Early and individualised physio intervention reduces the risk of chronic pain, enhances functional recovery and supports long-term self-management (Marrache et al., 2022).
Approximately 13% of women and 10% of men over 60 have symptomatic knee OA After age 70, prevalence increases to around 40% (Hawker, 2019)


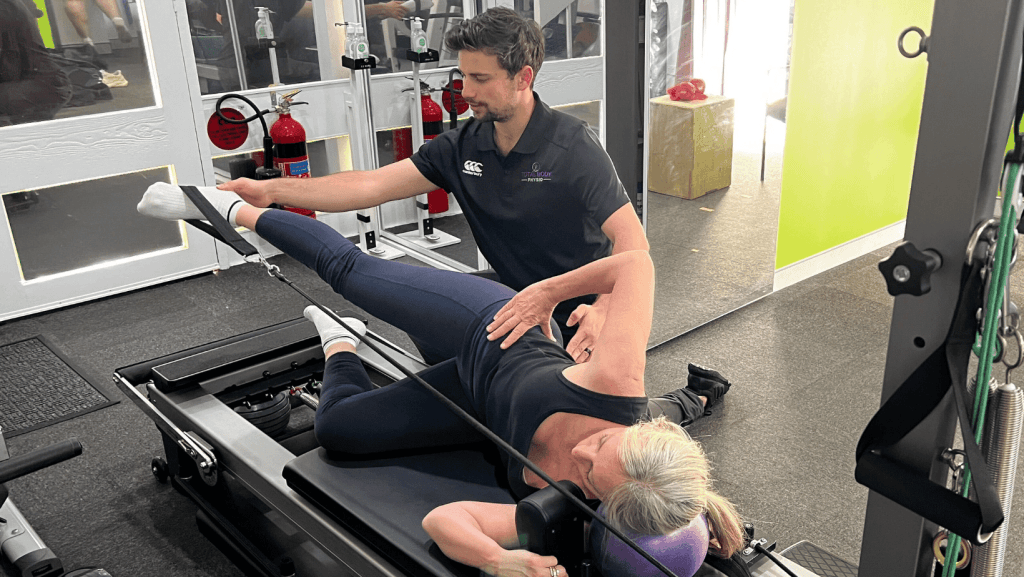
Why Clinical Pilates is So Effective?
Clinical Pilates led by our physiotherapists, is a form of exercise that focuses on restoring optimal movement through core stability, motor control, and neuromuscular re-education. It is distinctly different from generic Pilates classes, as it is tailored to the individual’s specific pathology and functional goals.
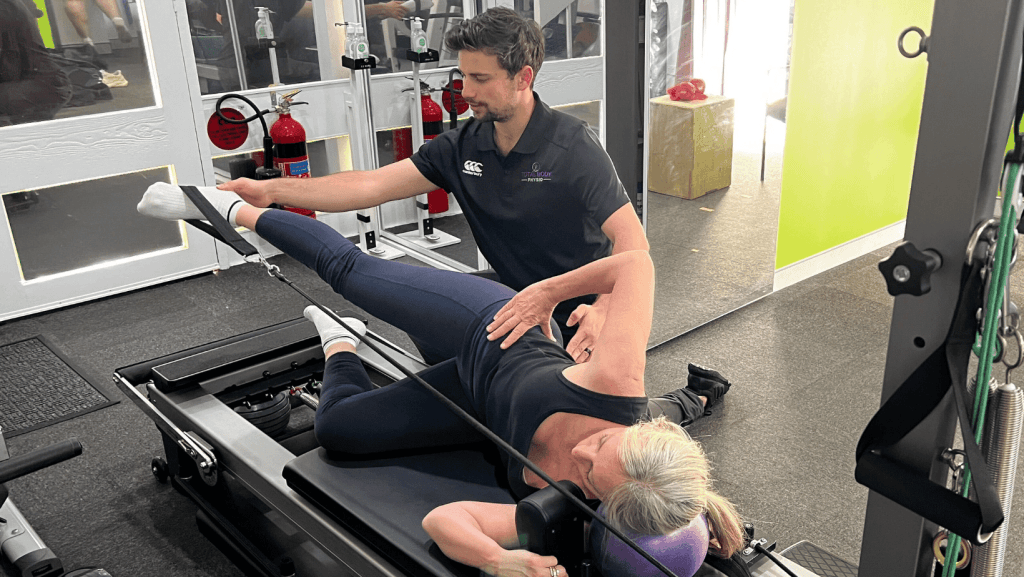
Robust research demonstrates that Clinical Pilates delivers significant benefits:
- Superior Pain Reduction and Functional Improvement: A 2020 systematic review concluded that Pilates is more effective than minimal intervention and equally effective as other forms of exercise for reducing pain and disability in chronic LBP, with benefits maintained at long-term follow-up (O’Neil et al., 2020).
- Targets the Root Cause: Studies using ultrasound imaging have shown that individuals with chronic LBP often have atrophy and poor activation of deep core muscles. Clinical Pilates specifically targets and improves the activation of these key stabilisers (transversus abdominis and multifidus), providing a foundation for a pain-free spine (Lin et al., 2021).
- Builds Movement Confidence and Reduces Fear: By providing a safe, supervised, and progressive environment, Clinical Pilates directly addresses kinesiophobia (fear of movement), which is a major predictor of chronicity. Patients regain trust in their body’s ability to move without pain (Huang et al., 2022).
- Enhances Proprioception and Corrects Movement Faults: LBP is often linked to poor proprioception and dysfunctional movement patterns. Pilates exercises retrain body awareness, posture, and coordinated movement, addressing these deficits across the entire kinetic chain (Shamsi et al., 2021).


Physio-Led vs Generic Pilates: A Critical Difference
Physio-led Clinical Pilates differs significantly from generic Pilates classes by being delivered by university-qualified physiotherapists who provide comprehensive assessments and tailor programs specifically for pain management and functional rehabilitation. Unlike general classes focused on fitness and flexibility, physio-led Pilates addresses individual injury history, movement deficits, and safety through supervised, progressive sessions that integrate with broader rehabilitation plans, ensuring a more effective and safe recovery for patients with lower back pain.


How is Clinical Pilates used in our clinic
For patients with back pain, Clinical Pilates is seamlessly combined with hands-on therapy, flexibility, strength training (often gym-based), and specific return-to-work or sport protocols. We prioritise restoring fundamental motor control and movement patterns before adding significant load, ensuring a resilient and sustainable recovery.
For those without a specific issue seeking Pilates in our clinic, a comprehensive One-on-One Initial Physio Assessment is essential. This comprehensive analysis of movement, motor control, strength, and stability allows our clinicians to create a fully individualised prescription targeting deficits assessed. Patients often begin with one-on-one sessions before progressing to our Small Supervised Group Classes of 4 participants, which ensure correct technique and optimal progression while maintaining individual attention.


Key Takeaways
- Early physiotherapy intervention, including Clinical Pilates, reduces the risk of acute LBP becoming chronic (Qaseem et al., 2020).
- Clinical Pilates provides superior improvements in pain and function compared to general exercise for chronic LBP patients (O’Neil et al., 2020; Lin et al., 2021).
- It is a safe, progressive, and effective long-term strategy for prevention and management of recurrent symptoms.
Our primary goal is to help our patients move better, feel stronger, and reclaim their lives without relying on medication or activity avoidance. For more information or to refer someone for a physiotherapy assessment or to our Clinical Pilates program in Five Dock or Summer Hill, please contact our clinic.
If you or someone you care for has an injury, a flare up, requires some rehabilitation or experiences an increase in pain, give the clinic a call on 9713 2455 or book online.