Rotator Cuff Tendinopathy
In Australia, shoulder pain affects up to 27% of the population under 70 years old annually (McKenna et al., 2025). At the heart of many shoulder problems is the rotator cuff, a group of muscles and tendons essential for shoulder stability and movement. When these tendons become overloaded due to factors like repetitive overhead activity, poor posture, or aging, rotator cuff tendinopathy can develop. This condition is a leading cause of shoulder pain and accounts for up to 70% of shoulder-related visits in primary care (Desmeules et al., 2025).

What is the Rotator Cuff?
The rotator cuff consists of four muscles and their tendons that surround the shoulder joint, connecting the shoulder blade (scapula) to the upper arm bone (humerus). Their primary function is to stabilise the shoulder by holding the “ball” of the humerus securely in the shallow “socket” of the scapula. These muscles also aid in rotating the arm inward and outward, as well as lifting it. Together, they provide both strength and stability to the body’s most mobile joint.
Understanding Rotator Cuff Tendinopathy
Rotator cuff tendinopathy refers to the degeneration, inflammation, or overload of one or more rotator cuff tendons, most commonly the supraspinatus. Symptoms typically include pain at the front of the shoulder, especially when lifting or reaching overhead. If left untreated, chronic tendinopathy can lead to partial or full-thickness tears, ongoing weakness, or changes in shoulder mechanics (de Oliveira et al., 2024). Recent imaging studies suggest that tendon structure and pain levels may improve within weeks of a structured physiotherapy strengthening program, even before obvious tendon changes appear on scans
(Nguyen et al., 2024).
Common Signs and Symptoms
- Pain with overhead activity, lifting, or reaching
- Pain radiating into the upper arm or shoulder region
- Night pain, especially when lying on the affected side
- Reduced or painful shoulder movement
- Weakness or fatigue when using the arm


Contributing Risk Factors?
- Repetitive overuse: Continuous overhead or load-bearing activity can cause microtrauma and tendon degeneration (Pozzi et al., 2022).
- Poor biomechanics or posture: Rounded shoulders, limited thoracic mobility, and poor scapular control increase stress on the rotator cuff (Yamamoto et al., 2015).
- Muscle imbalance or weakness: Weakness in the rotator cuff or scapular stabilisers reduces dynamic joint stability (Akhtar et al., 2021).
- Age and anatomical changes: Reduced vascularity, altered collagen, or acromial shape may predispose tendons to injury (Sripathi et al., 2024).
- Occupational and sporting demands: Overhead workers and athletes (such as tennis players, painters, and manual labourers) face higher risk (Riddervold et al., 2022).
- Systemic factors: Emerging evidence suggests metabolic conditions like diabetes and high cholesterol may contribute to tendon pathology (Abate et al., 2023).


Physiotherapy Assessment and Treatment
Our clinic adopts a comprehensive, evidence-based approach to management, aiming to address both symptoms and underlying contributing factors.
Assessment includes:
- Subjective evaluation: Identifying onset, aggravating activities, occupational demands, and patient goals.
- Physical examination: Assessment of range of motion, strength, scapular control, and posture.
- Special tests: To differentiate tendinopathy from impingement, bursitis, or cuff tear (Faber et al., 2024).
- Biomechanical and load analysis: Identifying faulty movement patterns or training errors.
- Objective strength testing: Using systems like the AxIT dynamometers to compare internal and external rotator strength and endurance


Physiotherapy Management and Rehabilitation
- Successful rehab focuses on progressive tendon loading, restoring full movement, improving muscle activation patterns, and rebuilding functional strength. Exercise remains the first-line, most evidence-supported intervention (Desmeules et al., 2025). Additional forms of treatment include:
- Pain Management: Manual therapy, soft tissue release, and ice are commonly used assisting with symptom reduction. Adjunctive modalities such as shockwave therapy (ESWT) can provide short-term pain relief and improved function (Khan et al., 2024). Corticosteroid injections may reduce pain and inflammation temporarily; however, studies show no long-term advantage over exercise-based physiotherapy (Schmitz et al., 2024).
- Restoring Range of Motion: Joint mobilisation, soft tissue releases, dry needling, thoracic mobility work, and targeted stretching improve movement efficiency, muscle tone and reduce compensatory patterns. Emphasis is placed on restoring scapulohumeral rhythm and coordination.
- Strengthening and Tendon Loading: Progressive resistance training is the cornerstone of recovery. A 2024 longitudinal study found that tendon thickness and function improved significantly after 6–8 weeks of graduated resistance exercise (Nguyen et al., 2024). Training includes isometric loading initially, progressing to isotonic and functional strengthening to enhance tendon capacity and endurance (Tavares et al., 2022).
- Postural and movement re-education: Optimising posture and ergonomics reduces shoulder stress. Education focuses on activity modification, ergonomic set up and restoring efficient movement mechanics.
- Kinetic chain and biomechanical integration: Healthy shoulders rely on the entire kinetic chain. Improving thoracic mobility, trunk stability, and lower limb strength supports load transfer and control. Weak core muscles and thoracic stiffness can impair shoulder activation and increase overload risk (Abdelmohsen et al., 2021).
Key Takeaways
Rotator cuff tendinopathy is a common but highly treatable condition, especially with early intervention. Current research consistently supports individualised, exercise-based rehabilitation as the gold standard in treatment (Faber et al., 2024; Nguyen et al., 2024) and while corticosteroid injections can provide short-term relief, they do not outperform exercise alone in achieving long term lasting benefits (Schmitz et al., 2024). Physiotherapy that combines targeted tendon loading, biomechanical correction, and functional integration offers the best chance for pain-free movement and preventing recurrence.


Exercises that can help Plantar Fasciopathy
TheraBand External Rotation (Neutral Position)
Aim: Strengthen external rotators
How: Attach a TheraBand to a door handle. With your elbow at your side (90° flexed), rotate your forearm away from your body, keeping the elbow tucked in. Return slowly.


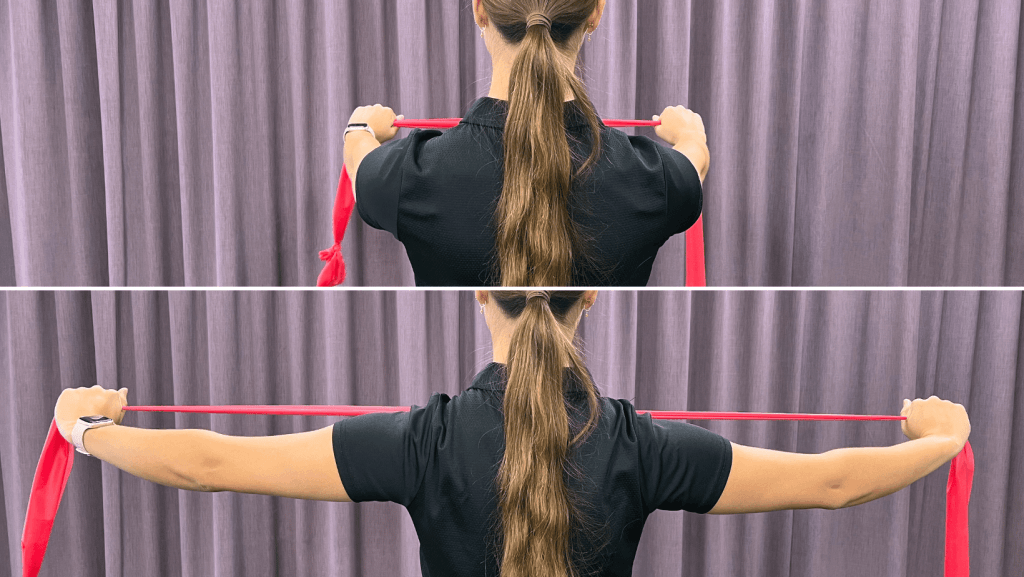
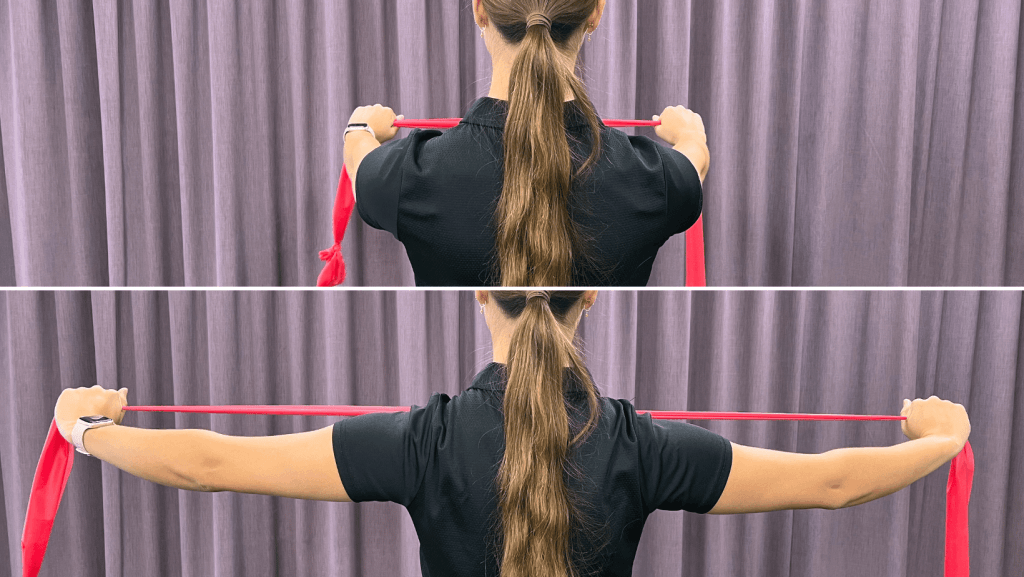
Banded Pull apart
Aim: Improve scapular control, posterior deltoid strength, and postural endurance.
How: Hold a band at shoulder height and pull apart, squeezing shoulder blades together. Hold 2–3 seconds; slowly release.
Pectoralis Stretch
Aim: Improve anterior shoulder flexibility, particularly Pectoralis major.
How: In a doorway, place forearm at 90°, gently lean forward until a stretch is felt in the chest. Hold 20–30 seconds.


If you or someone you care for has an injury, a flare up, requires some rehabilitation or experiences an increase in pain, give the clinic a call on 9713 2455 or book online.