Case study of the month: A path back to running after Achilles tendinopathy
Jared’s story
Jared is a 38‑year‑old recreational runner. He presented to Total Body Physio concerned as his “Achilles” was letting him down.
Around six weeks before his visit, Jared noticed a dull ache in the middle of his Achilles tendon. It was worst in the first ten minutes of running, on hills, and the morning after harder sessions. At the time, he had increased his training rapidly to prepare for a 10 km Christmas Fun Run.
As the weeks went on, Jared struggled to run more than 1–2 km before the tendon became sore and tight. Morning steps felt stiff and painful, and he noticed he could not push off properly when trying to run faster.
What we found
On assessment, Jared showed signs commonly seen in Achilles tendinopathy. These included localised tenderness through the mid-tendon, his calf strength was reduced on the affected side, single-leg calf raises were painful, and his ankle movement and gluteal stability were limited. There were no signs of tendon rupture, bursitis or other serious pathology.
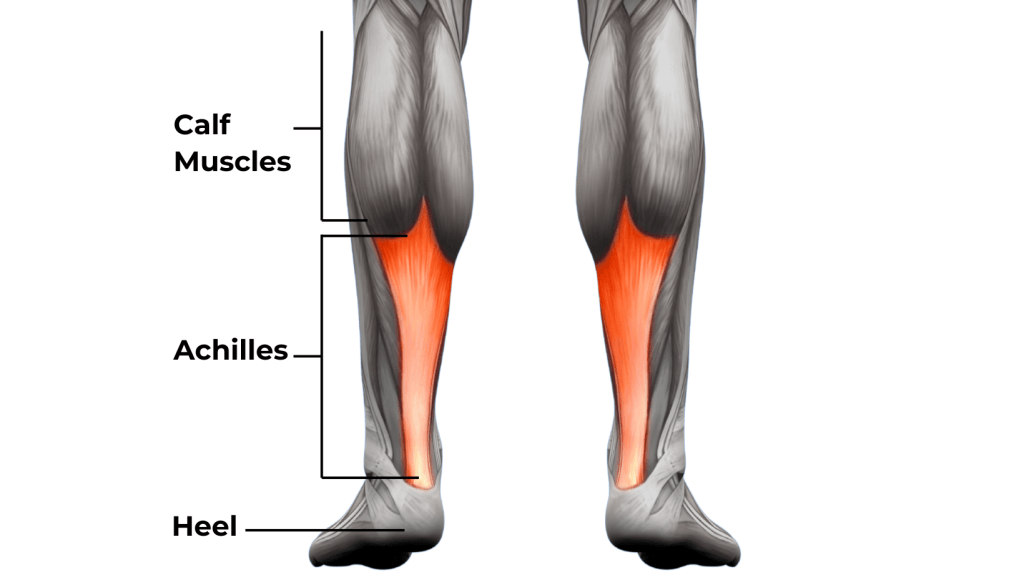
Understanding Achilles pain
The Achilles tendon connects the calf muscles to the heel bone and helps absorb and release force when we walk and run. During running, it works like a spring.
Mid-portion Achilles tendinopathy is common in runners. When training load increases too quickly, the tendon may struggle to keep up. It is often linked to a mismatch between the load placed on the tendon and its current capacity, particularly with activities such as hills, speed work, and higher training volumes (Maffulli et al., 2020). When the tendon is asked to do too much, too soon, changes may occur in how it handles load, leading to pain and stiffness.
Current tendon research describes a “continuum,” where symptoms and structural change sit on a spectrum and may improve with appropriate, graded loading rather than complete rest (Cook & Purdam, 2016).
Based on Jared’s history and examination findings, a diagnosis of mid-portion Achilles tendinopathy related to a rapid increase in running load was made, consistent with typical presentations described in the literature (Millar et al., 2021). Imaging was not required at this stage, as there were no red flags and symptoms were following an expected pattern.

The Plan
Jared’s rehab focused on improving tendon capacity rather than simply settling pain. Rehabilitation followed three key stages:
Phase 1 - Calm:
Running load was temporarily reduced. Isometric calf holds (holding a calf raise without movement) were introduced to provide stimulus to the tendon in a tolerable way. Research suggests that well‑tolerated isometric or slow, heavy loading can help manage tendon pain while starting the rehabilitation process. (Maffulli et al., 2020). We also worked on mobility and stability through the hips, core and lower limb and provided soft tissue massage to his overactive calf muscles and tight gluteals, and used Shockwave therapy as an adjunct to treatment. Evidence for extracorporeal shockwave therapy indicates that, when combined with an appropriate loading program, it may provide additional improvements in pain and function. (Paantjens et al., 2022)

Phase 2 - Build:
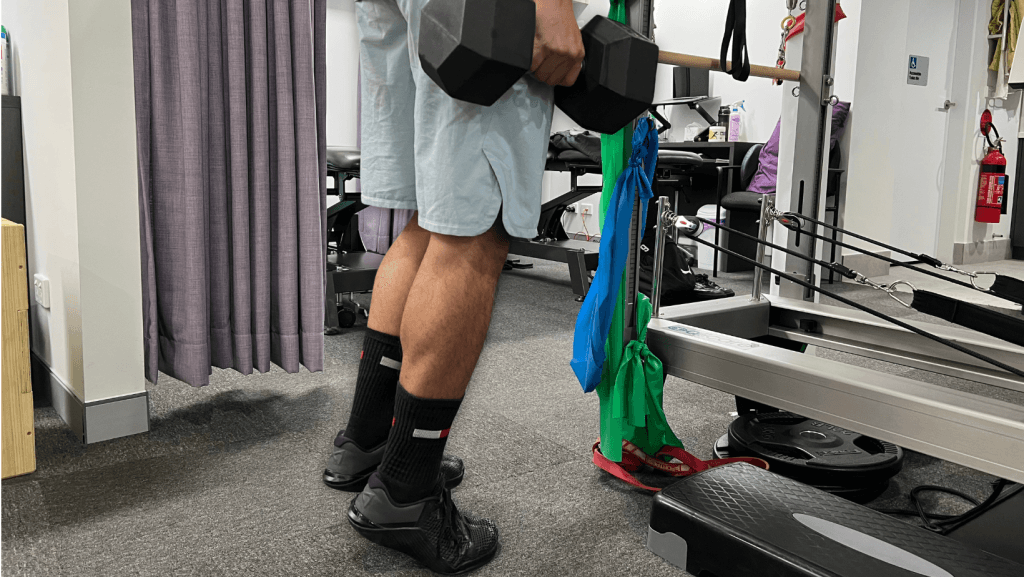
As symptoms settled, strengthening progressed with slow, controlled calf exercises to build tendon and muscle capacity, including variations to target both the gastrocnemius and the soleus muscles.
Research on mid‑portion Achilles tendinopathy supports progressive strengthening of the calf complex as a key driver of improvement in pain and function. (Pringels at el., 2025)
Jared’s lower limb strengthening program was progressed to gym based exercises including squats, lunges and deadlifts. Running was gradually reintroduced using a symptom-guided approach. Gait cues were introduced to improve running mechanics, such as a slightly shorter step and attention to how he pushed off during stance.
Phase 3 - Spring:
Later stages of rehab focused on restoring the tendon’s ability to store and release energy. Once Jared could tolerate good‑quality strength work with minimal symptoms, we began adding higher‑load activities and plyometrics including hopping, skipping, and running drills to prepare the tendon for higher loads and faster running.
Recent research supports staged, functionally based programs for chronicmid‑portion Achilles tendinopathy that integrate progressive strength and plyometric work, using criteria such as pain levels, calf‑raise endurance, and hop performance to decide when to advance or hold a phase. (Pringels et al., 2025) Running volume and speed were gradually increased as his tendon tolerated more load, with hill work and tempo efforts reintroduced nearer the end of this phase Jared continued his strength program throughout, as ongoing loading is important to maintain tendon health even after symptoms settle.

Tracking progress
Over eight weeks, Jared’s calf strength and running tolerance steadily improved.
Single-leg calf raises increased from 8 painful repetitions at the start, to 18 with mild discomfort by week 4, and 30 pain-free repetitions by week 8.

His running progressed from 1–2 km with pain, to 3 km more comfortably at week 4, and 6 km pain-free by week 8.
Objective testing in clinic using the AxIT Force Plates showed his affected calf strength improved from 70 percent of the other side at week 4 to 96 percent by week 8, with good symmetry on jumping and hopping tasks.

These measures reflect commonly used tools to track recovery in Achilles tendinopathy, including strength, function, and symptom response.


Outcome
By week 8, Jared was back running comfortably and working toward his 10 km Christmas Fun Run with a clear plan in place.
He also understood the importance of ongoing strength work to help reduce the risk of future flare-ups.
What Made the Difference
- Early accurate diagnosis
- Individualised progressive loading (Cook & Purdam, 2016)
- Strengthening both gastrocnemius and soleus
- Core and gluteal stability training & hip mobility work
- Correct timing of energy-storage (plyometric) progressions
- Adjunct therapies used strategically
- Symptom-guided return-to-running program
- Consistent home program with regular review
Take-home messages for runners
- Increase training gradually
- Keep calf strengthening as part of your routine
- Morning stiffness can be an early warning sign
- Ongoing pain may benefit from assessment and a structured rehab plan
If Achilles pain has been limiting your running or training, a clear diagnosis, physiotherapy rehabilitation and a progressive loading plan can help you get back on track.
If you or someone you care for has an injury, a flare up, requires some rehabilitation or experiences an increase in pain, give the clinic a call on 9713 2455 or book online.