Case study of the month: A Path Back to Sport After Chondromalacia Patellae
Patient: Alex, 26
Competitive basketball player Presenting issue: Persistent anterior right knee pain limiting training and competition

Alex’s Story
Three months prior to presentation, Alex developed gradual-onset knee pain during an intense period of basketball loading involving extra jumping drills and consecutive games but no acute traumatic incident was reported. Pain appeared with stair descent, deep squats, and eventually running, jumping, and even sitting. Self-management (ice, load reduction) gave only temporary relief. After a normal X-ray from his GP and ongoing pain affecting his performance and confidence, Alex sought physiotherapy.
Assessment Findings
- Reduced quadriceps strength, especially near full knee extension
- Decreased gluteal (hip) stability and strength
- Poor knee control on single-leg squat and landing tasks (“knee buckle”)
- Symptoms were reproduced with patellar compression and loaded bending
These findings aligned with common contributors to patellofemoral pain—quadriceps and hip weakness with altered movement control (Roth et al., 2022). Ligament and meniscal structures appeared intact, confirming a diagnosis within the patellofemoral pain spectrum (Collins et al., 2024).
An MRI was organised as Alex was extremely frustrated with how much his knee was affecting his basketball which revealed grade 2 chondromalacia patellae, meaning mild cartilage softening and superficial fissuring, but no full thickness loss. Such early-grade changes are often managed conservatively with good outcomes (Kothari et al., 2024)
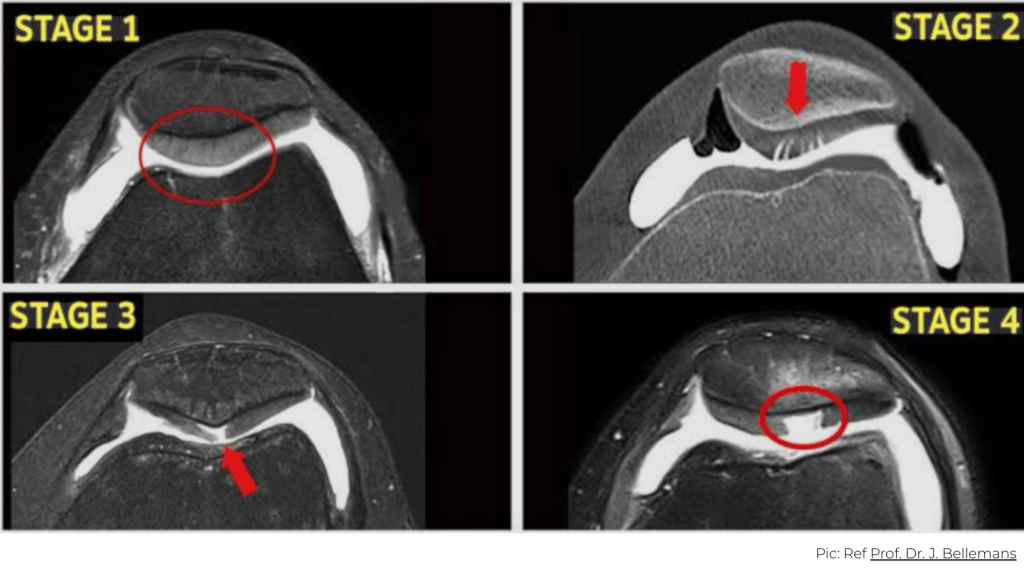
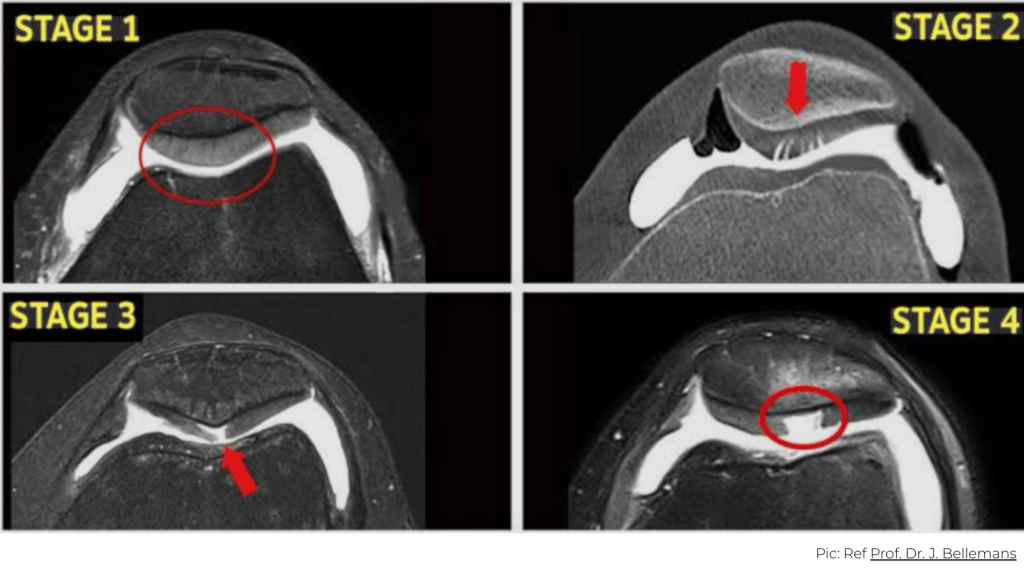
Understanding Chondromalacia Patellae
Chondromalacia Patellae refers to softening or fissuring of cartilage under the kneecap from repetitive stress on the patellofemoral joint. These structural findings don’t always correlate with pain, as symptoms often reflect load sensitivity rather than cartilage severity (Collins et al., 2024).
The condition is multi‑factorial and load‑related, driven by quadriceps and hip weakness, altered mechanics, and training spikes (McAlindon et al., 2022). Precisely what appeared in Alex’s case.
First-line treatment is conservative rehabilitation emphasising:
- Progressive quadriceps and hip strengthening
- Movement pattern and muscle activation retraining looking at the whole kinetic chain
- Gradual load exposure, and reintroduction to sport-specific demands and loads
Alex’s Rehabilitation Journey


Phase 1 – Settle Symptoms
Initial focus: symptom relief and movement maintenance. Manual therapy to settle symptoms and improve movement (massage, trigger point, and dry needling) complemented exercise programming. Adding manual therapy to hip/knee exercises significantly improves pain, function, and strength (Alkassab et al., 2025). Basketball load was modified (avoiding deep flexion and high-frequency jumping). Isometric quads and low-load hip/core work was prescribed to maintain strength, reduce symptoms, improve muscle activation and control, prioritising pain-guided loading over rest (Collins et al., 2024).


Phase 2 – Rebuild and Retrain
With symptoms reduced and task predictability improved, rehabilitation progressed to strength restoration and sport-specific performance. Controlled knee extensions, split squats, step-downs, and leg press were introduced within symptom-tolerant ranges. Emphasis was placed on hip abductor and external rotator strength to optimise knee alignment, supported by recent evidence that combined hip/knee programs were superior to knee-only exercises (Roth et al., 2022).
Neuromuscular retraining addressed control through single-leg squat, landing, and cutting mechanics, progressing to plyometrics, jumping, and basketball specific drills. Load was increased through volume, speed, and complexity using criteria-based progression to guide return to full training and competition (McAlindon et al., 2022).


Tracking Progress and Outcome
Over eight weeks, Alex demonstrated consistent improvements in strength, motor control, and symptoms:
- Pain-free single-leg squat by week 6
- Quadriceps strength symmetry improved from 82% to 97% by week 7 on AXIT strength testing.
- Single-leg hop distance increased by 18% on the affected side, with improved landing mechanics.
These outcomes align with key recovery markers for patellofemoral pain (Barton et al., 2023).
By week 8, Alex returned to full basketball training and match play with no post-session pain and renewed confidence. He continues a gym-based program to maintain long term knee health and prevent a recurrence.


What Made the Difference
- Accurate assessment, diagnosis and load management
- Progressive quadriceps and hip strengthening (Roth et al., 2022)
- Motor control and load retraining to reduce patellofemoral stress
- Gradual re‑exposure to jumping and landing demands
- Criteria‑based, progressive return‑to‑sport programming (McAlindon et al., 2022)
- Consistent exercise adherence and compliance with physiotherapy
Key Takeaways
- Anterior knee pain often reflects load intolerance and influenced by biomechanical factors rather than structural damage alone (McAlindon et al., 2022).
- Rest alone is rarely sufficient for chondromalacia patellae – active, guided rehabilitation produces superior improvements in pain and function (Roth et al., 2022).
- Strength, motor control, and progressive loading are key to recovery (Collins et al., 2024).
- Structured, evidence-based rehabilitation helps restore confidence and supports a safe return to sport (Kothari et al., 2024).
If you or someone you care for has an injury, a flare up, requires some rehabilitation or experiences an increase in pain, give the clinic a call on 9713 2455 or book online.