ACL Injuries: Your Guide to Prevention, Treatment & Recovery
What is the ACL?
The ACL (Anterior cruciate ligament) is one of the key stabilising ligaments of the knee connecting the femur (thigh bone) to the tibia (shin bone). It helps control forward movement of the tibia on the femur and rotation of the knee joint. The ACL stabilises the knee joint during cutting, pivoting, and rapid deceleration.
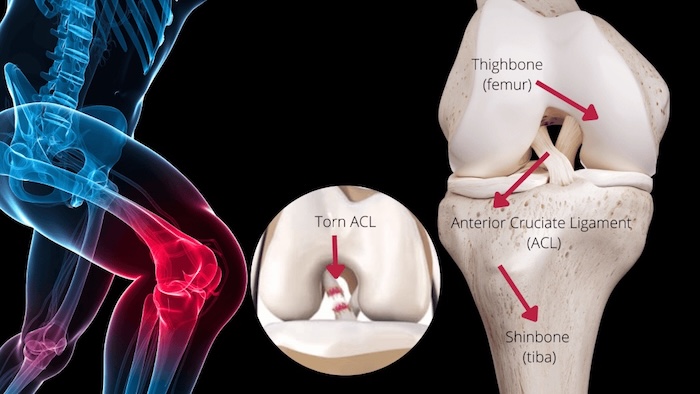
What is an ACL Injury?
An ACL injury involves a tear or rupture of this ligament. Injuries typically occur during sudden stops, changes of direction, or pivoting movements—often without contact.
These injuries often occur during non-contact actions like pivoting, sudden stopping or rapid directional changes and may be accompanied by damage to the menisci or MCL. Anterior cruciate ligament (ACL) injuries are common and serious, particularly in active individuals and athletes in sports like netball, soccer, skiing, AFL, basketball, and rugby (Allot et al., 2022). Without proper rehabilitation, ACL injuries can lead to knee instability, reduced function, and early osteoarthritis (Davis et al., 2021).
What is an ACL Injury?
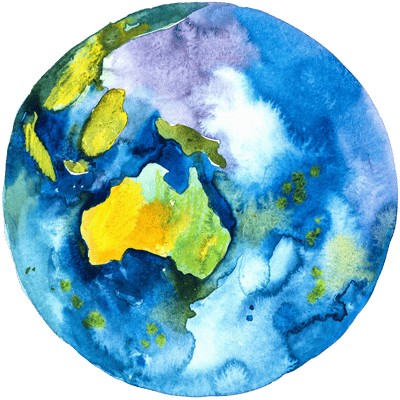
Australia has the highest rate of ACL reconstructions globally, especially in young adults (Vertullo et al., 2018).


ACL injuries have increased by 75% in under-25s over the past 20 years (Smith et al., 2023)


Females are 2–8 times more likely to sustain an ACL injury than males in the same sports (Macmillan, 2020).


1 in 3 young athletes re-injure their ACL within 2 years of returning to sport (Hughes et al., 2020).
Common Risk Factors
- Sudden changes in direction or poor landing mechanics (Johnson et al., 2022)
- Quad dominance and weak glutes or hamstrings (Lee et al., 2023).
- Previous ACL injury (Brown et al., 2023).
- Poor single-leg balance or neuromuscular control (Smith et al., 2022).
- Inadequate sleep (<8 hrs increases injury risk by 70%) (Miller et al., 2023)
- Hormonal factors, including estrogen-related ligament laxity (Anderson et al., 2023).
Diagnosis / Assessment:
Physiotherapists are experts at diagnosing knee injuries, and our physio team are highly competent in diagnosing ACL injuries. Subjectively the patient will typically describe an incident followed by a “pop”, immediate swelling, instability or the knee “giving way” when walking, and difficulty weight-bearing. Common physical assessment findings that indicate an ACL rupture include:
- Positive Lachman’s test (no end feel), pivot-shift test and anterior drawer
- Reduced knee ROM in flexion & inability to fully straighten the knee.
- Knee joint effusion & swelling
- Lateral joint line tenderness: “In patients with ACL rupture there is an 85% probability of concurrent associated bone bruising at the femoral condyle or tibial plateau (Lee et al., 2023)
- Confirmation of an ACL tear occurs via MRI (which will also look for other coexisting injuries including MCL/LCL tears, meniscus tears, or impaction fractures).


Surgical vs Non-Surgical Management
The decision on whether surgery is required or not, depends on knee stability (is it giving way), other associated injuries, the patient’s age and lifestyle, and their functional and sporting goals.
Non-surgical rehab can be effective for individuals with partial tears or lower activity demands (Saueressig et al., 2022). Surgery is often recommended for young, active patients or those with high-grade tears and significant instability.
Collaborative decision-making between the patient and orthopaedic surgeon with input form the physio is essential to determine the best course of action.
The Importance of Immediate Physiotherapy Management
Physiotherapy is essential in ACL tear recovery, whether managed surgically or non-operatively. Early rehabilitation—immediately after injury—helps prevent muscle loss and abnormal movement patterns. Initial goals include reducing swelling, restoring knee motion, normalising gait, and activating the quadriceps.
Evidence also supports physiotherapy both before and after surgery to improve outcomes and reduce graft failure risk. Failla et al. (2016) showed that 10 pre-op sessions improved knee function and return-to-sport rates, while Grindem et al. (2016) found a five-week pre-op strengthening program led to better two-year outcomes. Johnson et al. (2022) reported that early physiotherapy reduces complications and speeds up recovery, reinforcing the importance of early intervention.


Conservative Rehabilitation
If surgery is not required, the rehabilitation process continues progressively to ensure full movement and function is achieved. Rehabilitation involves restoring strength and neuromuscular control, improving balance and proprioception, and advancing towards agility, plyometric exercises, and activity-specific or sports-specific training.


Physiotherapy Rehabilitation After ACL Reconstruction
Physiotherapy is crucial after ACL surgery to regain strength, movement, return full function and prevent re-injury. Rehabilitation goals through the different phases include:
- 0–2 Weeks: Reduce pain/swelling, improve VMO activation, restore extension, normalise gait.
- 2–6 Weeks: Regain motion, improve muscle function, begin proprioception and neuromuscular control training.
- 6–12 Weeks: Build strength throughout lower limb, improve single-leg control, improve proprioception, and introduce low-level plyometrics
- 12–24 Weeks: Progress to heavy resistance, advanced neuromuscular drills, and begin running.
- 6–9 Months: Focus on sport-specific drills, agility, and continued strengthening.
- 9+ Months: Prepare for return to sport with game-like and neurocognitive training.
Throughout recovery in our clinic strength testing is performed using the AxIT dynamometers and force plates, helping us gauge strength gains and deficiencies, imbalances and asymmetries. This helps guide recovery, programming and assists with a safe return to sport and activity.


Return to Sport After ACL Surgery
Returning to sport after ACL reconstruction should be based on individual progress and meeting key criteria, not just time since surgery. Re-injury risk is highest within the first two years, particularly in the early stages after return. In fact, delaying return to sport until after 9 months can reduce the risk of re-injury by over 50% each month delayed (Grindem et al., 2016). Recent studies have further supported the benefits of a delayed return; for instance, a 2023 study by Nagelli et al. demonstrated that waiting at least 12 months post-surgery before returning to high-intensity sports decreased the likelihood of re-injury by 60%, emphasizing the importance of patience and thorough rehabilitation.
Return-to-Sport Requirements
- Quad strength ≥ 90% of the uninjured leg
- Hop and agility test symmetry ≥ 90% of the uninjured leg and passes normative data scores
- Confidence in movement and decision-making under fatigue
- Psychological readiness (e.g., high ACL-RSI score)
- Completed sport-specific training and deceleration drills
- Athletes who return before meeting these criteria are more likely to suffer re-injury, with rates as high as 1 in 3. Long-term neuromuscular training and gradual return are essential to protect the graft and future performance. (Beischer et al., 2020)


Tips to Preventing ACL Injury or Re-Injury
Up to 50% of ACL injuries are preventable with the right strategies (Sadoghi et al., 2012). Consistent neuromuscular training and technique-focused warm-ups significantly reduce injury risk.
- Strengthen Key Muscles: Focus on quads, hamstrings, hips, and core to stabilise the knee.
- Balance and Stability: Improve single-leg control for better landing and injury prevention.
- Safe Movement Patterns: Land softly, keeping knees aligned with toes to avoid inward collapse.
- Plyometric Exercises: Use explosive movements to boost knee stability and neuromuscular control.
- Recovery and Nutrition: Prioritise sleep (8+ hours) and nutrition for tissue health and injury prevention (Milewski et al., 2014).
- FIFA 11+ Program: A 15–20 min specific warm-up like the FIFA 11+ program reduces ACL injuries by 30–50% (Sadigursky et al., 2017).


If you or someone you care for has an injury, a flare up, requires some rehabilitation or experiences an increase in pain, give the clinic a call on 9713 2455 or book online.