What is Plantar Fasciopathy?
Plantar fasciopathy, sometimes referred to as plantar fasciitis, describes localised pain at the plantar fascia insertion onto the calcaneus (heel) caused by overload in the fascial tissue. It is now understood as a degenerative condition involving microtears and collagen disorganisation rather than purely inflammation (Nweke et al., 2025). It is the most common cause of heel pain in adults and typically presents with pain that is worse during the first steps in the morning or after rest (Morrissey et al., 2021).
What is the Fascia?
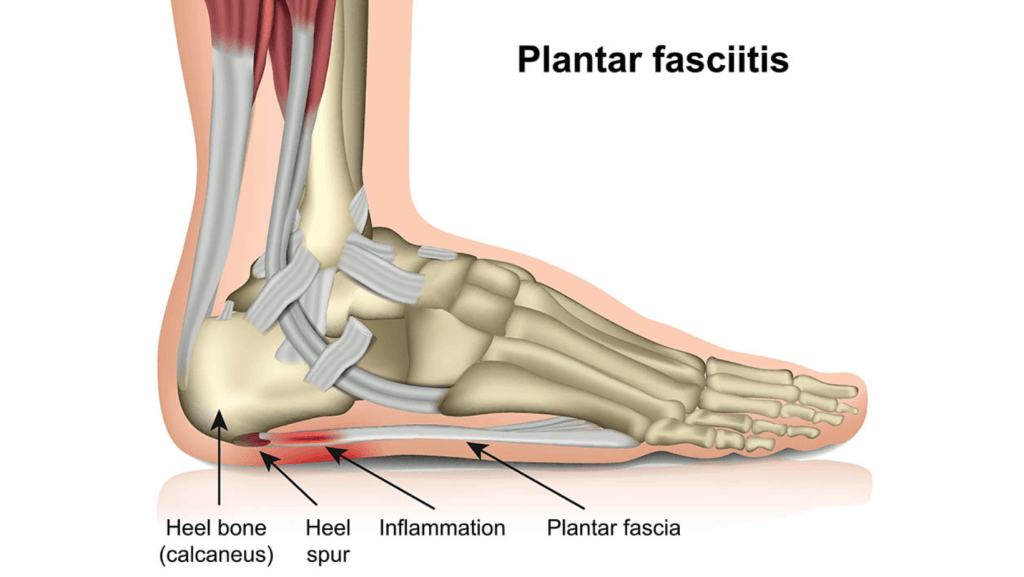
Fascia is a thin yet strong layer of connective tissue that surrounds and supports your muscles, bones, nerves, and organs. It helps hold everything in place while still allowing movement. Composed primarily of collagen, fascia helps transmit forces throughout the body and plays an important role in stability and coordination. The plantar fascia is a thick, strong band of this tissue that runs along the bottom of your foot, from the heel bone (calcaneus) to the base of your toes. It supports the arch of the foot and acts like a natural shock absorber every time you walk, run, or stand.
Causes of Plantar Fasciopathy
- Repetitive strain and overload on the plantar fascia from excessive or altered physical activity and prolonged standing (Di Caprio et al., 2023; Haley, 2021).
- Biomechanical issues like overpronation, gluteal weakness and tight calf muscles increase stress on the plantar fascia (Nweke et al., 2025).
- Reduced ankle dorsiflexion (toes back towards your head) limits normal foot motion, transferring extra load to the fascia (Sullivan et al., 2015).
- Obesity and aging contribute to higher mechanical load and decreased tissue resilience, making the plantar fascia more prone to injury (Rassenburg et al., 2022).
These factors individually or combined increase tensile forces on the fascia leading to microdamage and plantar fasciopathy (Koc Jr. et al., 2023).
Diagnosing Plantar Fascia Pain
Diagnosis of plantar fasciopathy is based on a detailed history and physical examination. Patients typically report pain under the heel, often worse with the first few steps in the morning or after periods of rest. It may improve slightly with movement, then worsen again after prolonged activity. On examination there is:
- Pain on Functional Plantar Flexion: Pain during single-leg calf raises is a useful clinical sign (Davenport et al., 2023).
- Tenderness on Palpation: Presence of tenderness over the medial calcaneal tubercle and plantar fascia origin helps localise the pathology (Nweke et al., 2025).
- Restricted Range of Motion: Limited ankle dorsiflexion and big toe extension are commonly found in affected patients (Lee et al., 2021).
- Windlass Test: A positive Windlass test, causing pain when dorsiflexing the big toe, confirms plantar fascia involvement (Martin et al., 2023).
- Biomechanical Assessment: Poor control at the hip or knee causing valgus collapse can increase foot pronation and strain on the plantar fascia (Morrissey et al., 2021).


How Do We Treat It?
Physiotherapy is fundamental to managing plantar fasciopathy. It focuses on reducing pain, stretching, strengthening, education, load management and correcting the underlying factors that caused the injury.
- Reduce irritation and improve mobility: Relative rest, gentle stretching, supportive footwear and taping to offload the heel. We often use manual therapy techniques to improve mobility through the ankle and foot joints, reducing excessive strain on the fascia.
- Load Management & education: Modifying activity levels, such as reducing training load and volume, or simply reducing step count, then using interventions such as taping, moonboots in severe cases, or footwear changes and orthotics to reduce plantar fascia stress is imperative (Lim et al., 2023).
- Progressive loading & Strengthening: Plantar fascia-specific exercises are known to have better outcomes. We will target the calf, the toe flexors and tibialis posterior. Strengthening foot intrinsic and lower limb muscles improves function and reduces disability (Koc Jr. et al., 2023).
- Improving biomechanics & muscle activation patterns: Abnormal biomechanics and poor muscle activation patterns are often the underlying causes of plantar fasciopathy. By correcting muscle activation patterns and improving lower limb alignment, we reduce the mechanical load on the plantar fascia, allowing it to heal while simultaneously preventing future overload and re-injury. (Lee et al., 2020; Harutaichun et al., 2021)
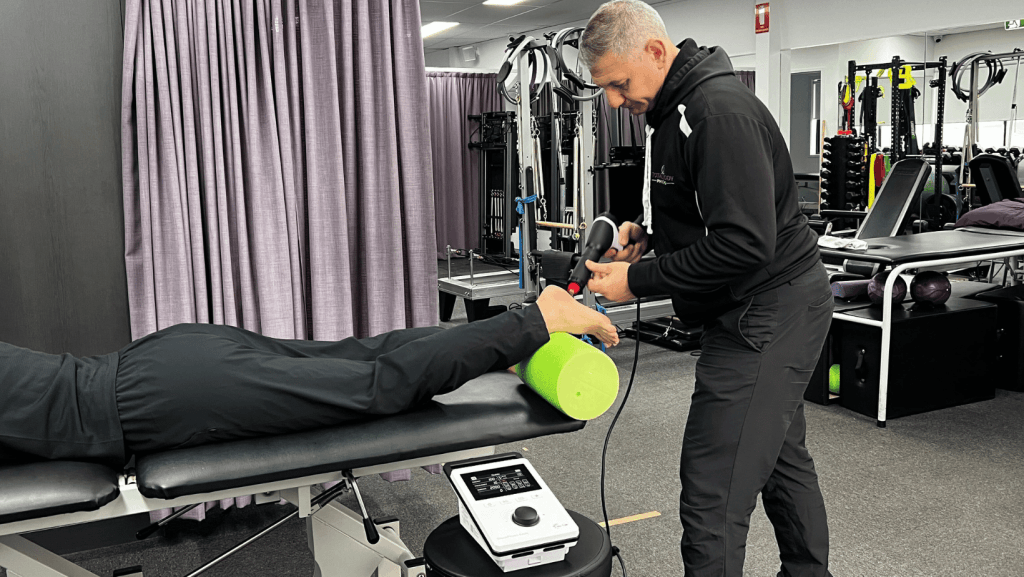
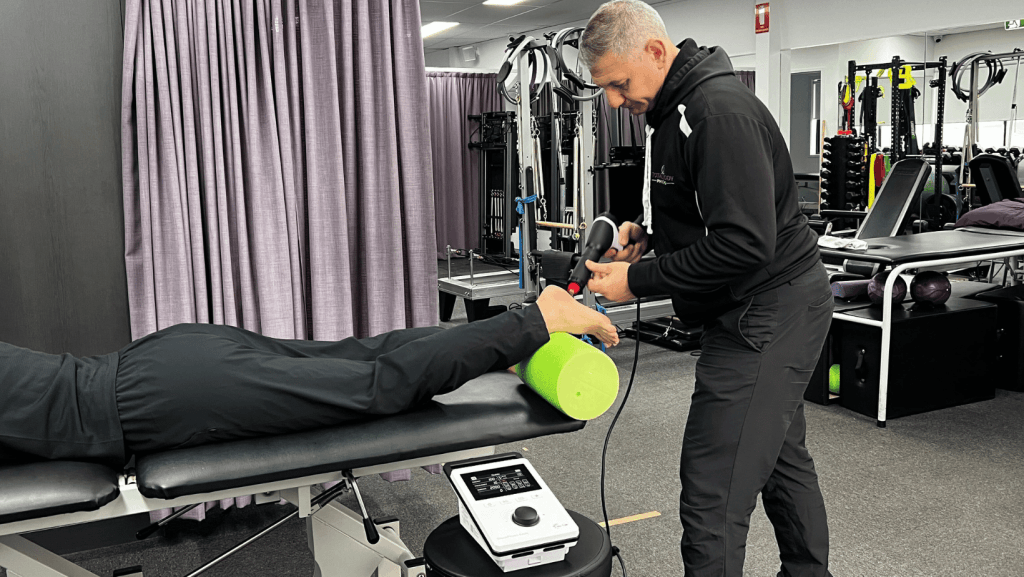
- Shockwave therapy, dry needling, or other adjunct treatments may be used for persistent cases to stimulate healing. (Karam et al., 2022; Morrone et al., 2022). We have access to both of these modalities in our clinic, and staff are fully trained in their use.
During rehabilitation, it is critical that we consider the patient’s functional and lifestyle goals. This approach ensures we not only reduce pain and symptoms, but also build a rehabilitation program that facilitates a return to their specific activities while reducing the risk of recurrence issues. We also use objective testing including the AxIT strength testing equipment to ensure adequate strength and force is produced in specific muscle groups such as the calf and the toe flexors, but also muscles further up the kinetic chain like the glutes.
Prevention of Plantar Fasciopathy
- Gradual progression in physical activity: avoiding sudden increases in running volume or spikes in load is essential to prevent overuse of the plantar fascia. (Riel et al., 2023).
- Maintaining a healthy body weight: higher body mass index (BMI) increases plantar fascia strain, contributing to the onset and recurrence of plantar fasciopathy (McPoil et al., 2023).
- Wearing supportive footwear: footwear with good arch support, heel cushioning, and motion control features reduces stress on the fascia (Umar et al., 2022).
- Strengthening of foot and calf muscles: strength training is a key pillar in both prevention and recovery of plantar fasciopathy (Lima et al., 2024).
- Addressing biomechanical inefficiencies early: abnormal foot posture, overpronation, and limited ankle dorsiflexion are modifiable risk factors (Riel et al., 2023).


Exercises that can help Plantar Fasciopathy
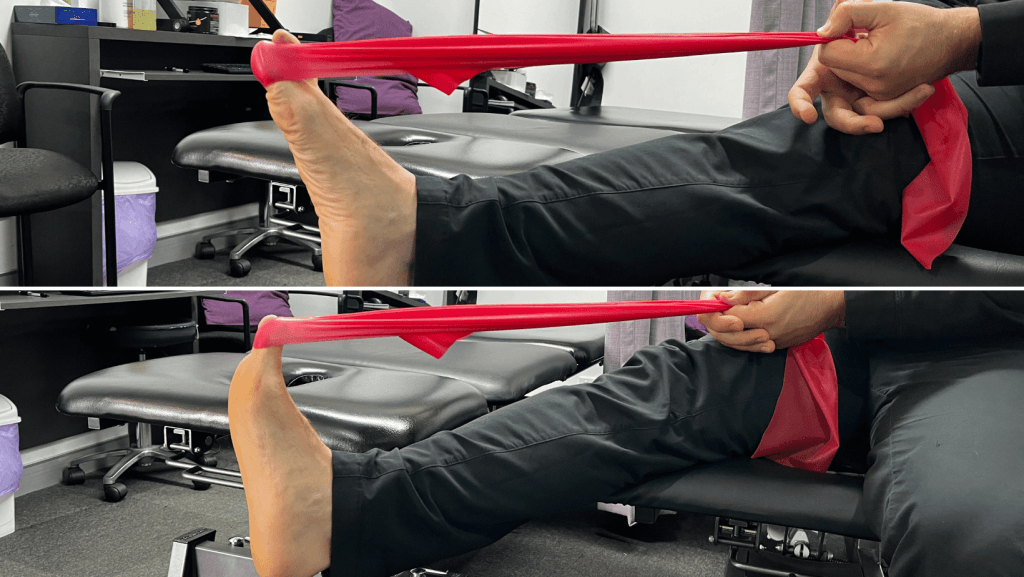
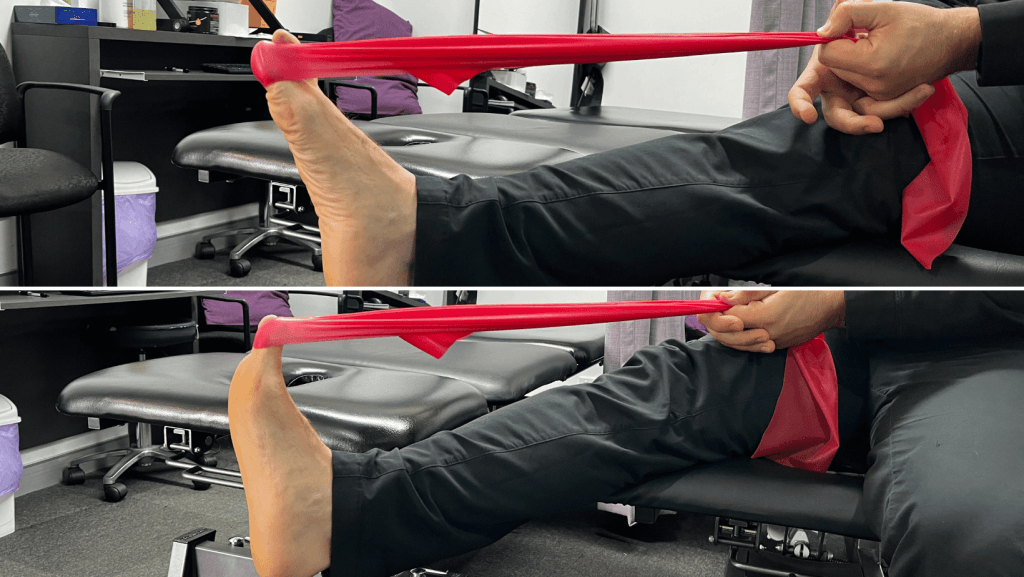
Big toe flexion
Aim: Big toe flexion exercises strengthen the muscles that support the arch, improve the efficiency of walking and running, and help manage pain during the push-off phase. By strengthening the toe flexors and peroneal muscles, the stress on the plantar fascia is reduced, which can help with healing and pain prevention (Kamonseki et al., 2016).
How: Loop a band around your big toe, hold the ends, and pull your big toe up against the band, then press it back down against the resistance.
Spikey ball self release
Aim: Spikey ball massage serves multiple purposes in managing plantar fasciopathy. It helps reduce pain by stimulating nerve receptors that block pain signals, improves tissue flexibility by releasing adhesions in the plantar fascia, and increases blood flow to promote healing. This simple, effective self-treatment tool empowers patients to actively manage their symptoms and maintain flexibility between physiotherapy sessions.
How: Sit in a chair with the spikey ball under your foot, positioned at the heel where the plantar fascia attaches. Apply moderate pressure and slowly roll the ball from your heel toward your toes, pausing on any tender points for 30-60 seconds. Work across the entire width of the plantar fascia, avoiding excessive pressure that increases pain. This can be done 1-2 times a day.


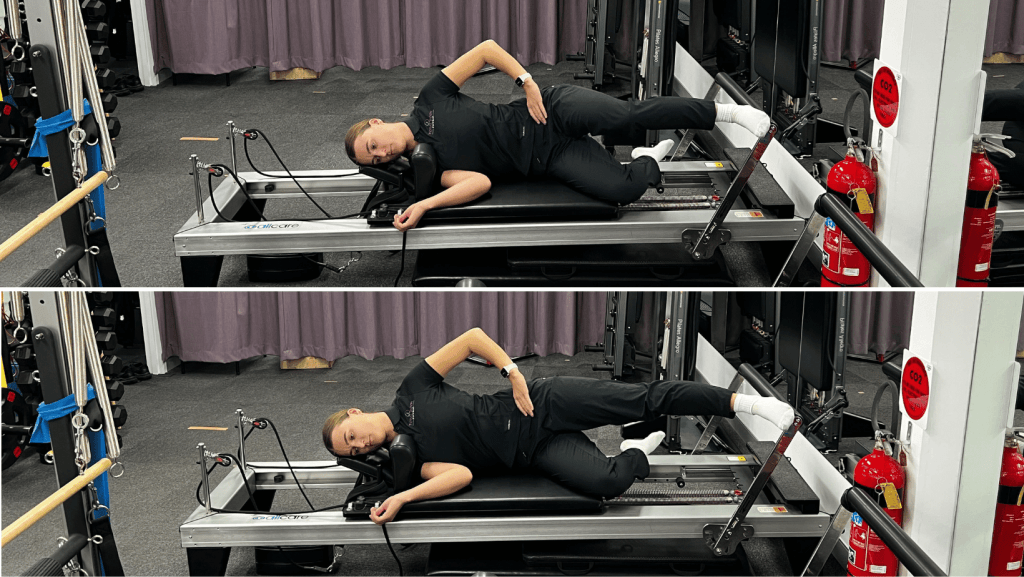
Side-lying Single leg Squat on reformer
Aim: Improve Gluteus Medius stability & endurance. This reformer exercise targets hip strength and control – a critical component often overlooked in plantar fasciopathy management. Weak hip abductors can lead to poor knee and foot alignment (valgus buckle), increasing pronation forces and strain on the plantar fascia. By strengthening the gluteal muscles in a controlled, progressive manner, we address these proximal biomechanical deficits and reduce load on the plantar fascia, setting the foundation for pain-free movement.
How: Lying on your side on the reformer with your hips facing forward, place the top leg on the foot bar parallel to the ground. Press through your heel to straighten the top leg, pushing the carriage away, then slowly control it back to the starting position. Ensure that your knee stays in line with your second toe (or lifts up towards the sky) as you squat to further target your gluteus medius. Level of difficulty can be adjusted by changing spring resistance.
If you or someone you care for has an injury, a flare up, requires some rehabilitation or experiences an increase in pain, give the clinic a call on 9713 2455 or book online.