Understanding Shin Splints
What are Shin Splints?
Shin splints, medically known as Medial Tibial Stress Syndrome (MTSS), describes pain along the inner edge of the shinbone (tibia). This condition commonly affects individuals who rapidly increase their training volume such as runners or those starting a new exercise routine.
The pain results from repeated stress on the tibia, which leads to irritation of the tissue covering the bone called the periosteum. The continuous tractional forces exerted by the attached muscles leads to inflammation, a bone stress response and microdamage to the cortical bone. This is particularly associated with the traction stress of the soleus, tibialis posterior and flexor digitorum longus muscles (Toh et al., 2022; Winters et al., 2021).


Prevalence of Shin Splints
- MTSS affects up to 13–20% of runners, particularly novice athletes who lack the musculoskeletal conditioning required to absorb repeated tibial loading (Hamstra-Wright et al., 2021).
- Female athletes are at a significantly higher risk due to a combination of biomechanical, endocrine, and nutritional factors such as relative energy deficiency, increased joint laxity and altered neuromuscular control (Kliethermes et al., 2022).
- In military settings, especially during initial physical training phases, the prevalence can be as high as 35%, reflecting the intense and rapid increase in load common in these environments (Newman et al., 2021).
Causes of Shin Splints
Shin splints are not due to a single factor, but can result from a combination of mechanical overload, muscular dysfunction and tissue fatigue. Key contributors include:
- Sudden increases in training volume or intensity that outpace the ability of the tibial cortex to remodel and adapt, causing stress to accumulate at the periosteum and underlying bone (Hamstra-Wright et al., 2021).
- Hard training surfaces like concrete or synthetic tracks can reduce shock absorption and increase the ground reaction forces transmitted through the lower limb.
- Poor footwear especially worn-out running shoes or those lacking medial arch support can increase impact and lead to biomechanical compensations that stress the tibia.
- Overpronation during gait causes excessive tibial internal rotation, creating torsional stress along the tibial shaft (Toh et al., 2022).
- Muscle tightness, particularly in the calf muscles, limits ankle dorsiflexion and alters gait mechanics, contributing to overload of the deep posterior compartment.


Risk Factors of Shin Splints
There are several intrinsic and extrinsic risk factors that predispose individuals to develop shin splints.
- Female gender: Higher risk is linked to lower bone mineral density, hormonal factors like menstrual dysfunction, and neuromuscular differences affecting load tolerance.
- Foot posture abnormalities: Flat feet or excessive navicular drop can cause overpronation and more tibial torsion when walking.
- History of MTSS or previous lower limb injury: Unresolved biomechanical issues or poor rehab increases the chance of recurrence.
- High BMI: Increases axial load on the tibia during weight-bearing activities, elevating the risk of bony stress.
- Calf tightness or weakness limits ankle dorsiflexion, changing gait and decreasing shock absorption, which increases load on the medial tibia.
- Poor neuromuscular control: Weakness in proximal hip stabilisers, particularly the gluteals compromises single-leg control and increases lower limb loading variability during repetitive tasks like running.


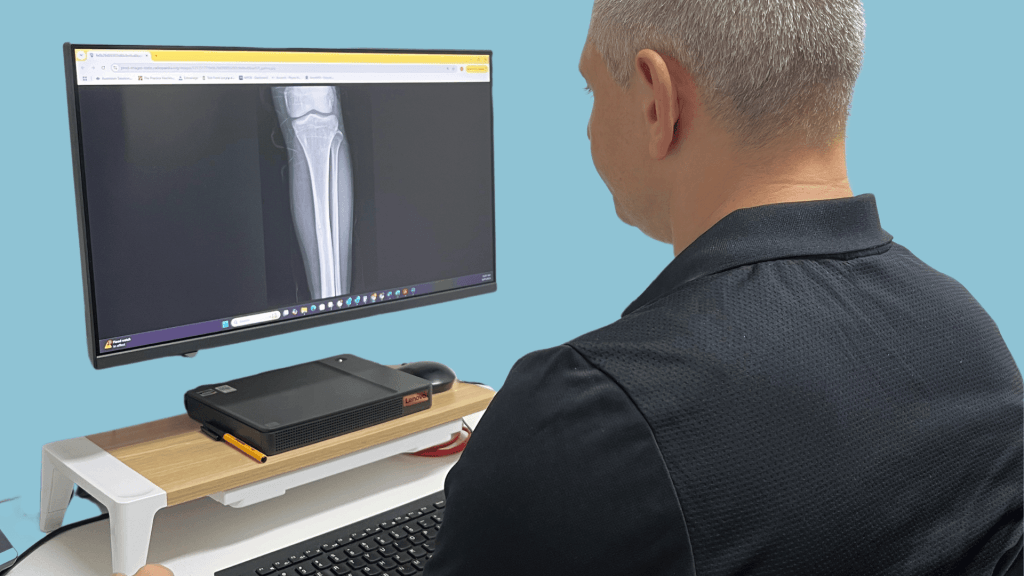
The Shin Splints Continuum
The continuum of shin splints begins with Medial Tibial Stress Syndrome (MTSS), characterised by diffuse, exercise-induced pain along the posteromedial border of the tibia due to repetitive traction and bone overload. If not managed, MTSS can progress along a spectrum of bone stress injury (BSI), culminating in a tibial stress fracture marked by focal pain, swelling and positive imaging findings (Miller et al., 2023). Early MTSS often presents without structural damage, but continued loading leads to microdamage, periosteal inflammation and cortical disruption indicative of a stress reaction or fracture (Snyder et al., 2023). Prompt diagnosis and load management are crucial to prevent progression.
Common Symptoms & Diagnosis
MTSS typically presents as exercise-induced, diffuse pain along the lower two-thirds of the medial tibia. The pain develops gradually with training and may persist post-exercise in more advanced cases. Tenderness is typically palpated along a broad (>5cm) area of the medial tibial border, without the localised focal pain that is characteristic of stress fractures. It often presents bilaterally, although severity may differ between legs.
Functional assessment frequently demonstrates pain provocation with single-leg hopping, repeated dorsiflexion against resistance, or impact activities such as jogging on the spot. Passive and active ankle dorsiflexion may elicit discomfort, especially when combined with inversion or resisted plantar flexion. Calf muscle tightness (particularly the soleus) and weakness of the deep posterior compartment of the lower leg and deep hip stabilisers may also be evident on strength testing.
Biomechanical evaluation may identify overpronation of the foot during midstance, flattening of the arch, or excessive navicular drop, all of which contribute to altered lower limb kinetics associated with MTSS.


The Role of Physiotherapy in Recovery
Physiotherapists play a key role in both recovery and patient education by applying an evidence-based approach to load management, rehabilitation, and return to sport:
- Relative rest: Physiotherapists reduce axial stress by modifying training loads while maintaining cardiovascular fitness through low-impact activities like swimming or cycling (Willy et al., 2020).
- Manual therapy: Soft tissue techniques including massage and dry needling are used to address muscular tightness in the calf and posterior chain (Collins et al., 2021).
- Progressive strengthening: Individualised strength programs targeting the soleus, tibialis posterior, foot intrinsics and gluteal muscles improve lower limb load distribution, overall biomechanics and functional control (Reinking et al., 2023).
- Gait retraining: An analysis of gait enables physiotherapists to adjust cadence, stride length and foot strike patterns to lower tibial stress during running and loading (Napier et al., 2021).
- Footwear and orthotics: Based on individual gait assessment, physiotherapists may recommend supportive footwear, prescribe orthoses or refer to a podiatrist to reduce medial tibial traction forces (Bonanno et al., 2022).
- Graded return to running: Structured return to sport programs tailored to individual recovery, ensuring tissue tolerance is restored before full activity is resumed. (Tenforde et al., 2020).


Prevention of Shin Splints
Preventative strategies focus on controlling mechanical load and improving lower limb resilience. Key strategies include:
- Load Management: Training volumes should increase gradually, ideally by no more than ≤10% per week with planned periods of reduced load to allow bone adaption and avoid overload injury risk (Afonso et al., 2023).
- Strength Training: Strengthening the calf complex, foot stabilisers and proximal hip muscles improves dynamic single leg control and reduces the risk of overload (Becker et al., 2024).
- Running Retraining: Gait retraining to increase cadence and reduce overstriding reduces impact forces and shear stress on the tibia (Davis et al., 2023).
- Footwear Management: Shoe selection should be guided by foot posture and gait mechanics and shoes should be replaced regularly to maintain support (Chan et al., 2023).
- Cross-Training: Incorporating low-impact cross-training like cycling or deep water running assists in maintaining aerobic fitness without overloading bone during offloading periods (Hoffman et al., 2024).
- Female Athlete Monitoring: Screening for RED-S (Relative Energy Deficiency in Sport) and menstrual irregularities is essential for preventing bone stress injuries in female athletes
- (Mountjoy et al., 2023).
Wall sit Soleus Raise


Aim: Build muscle strength in the Soleus Muscle to support the calf in bent-knee positions such as running and jumping while also isometrically working the quadriceps.
How: Using a wall, slide down into a wall sit position. While holding this position with knees bent, simply raise up and down on your toes targeting your soleus.
Arch Raises
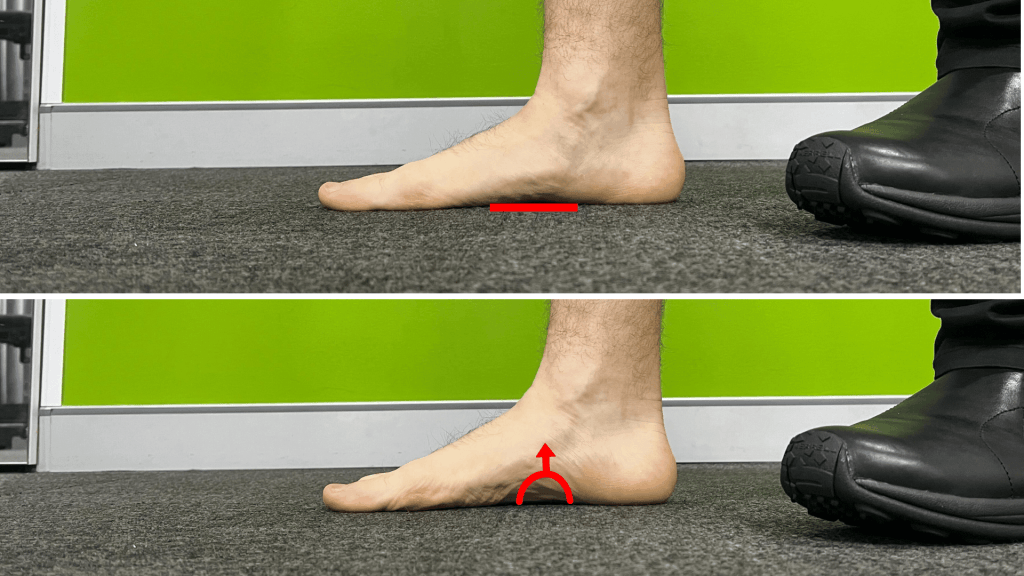
Aim: To activate tibialis posterior and the intrinsic foot muscles.
How: Standing with your foot flat on the ground, actively lift the inside arch of the foot. Hold 5 seconds and repeat.
SL squat on Reformer
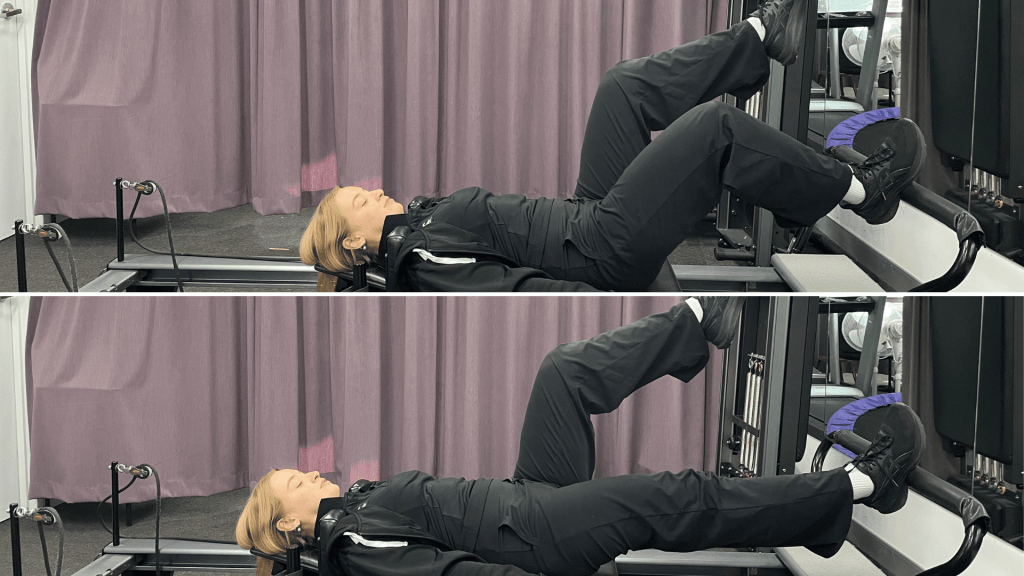
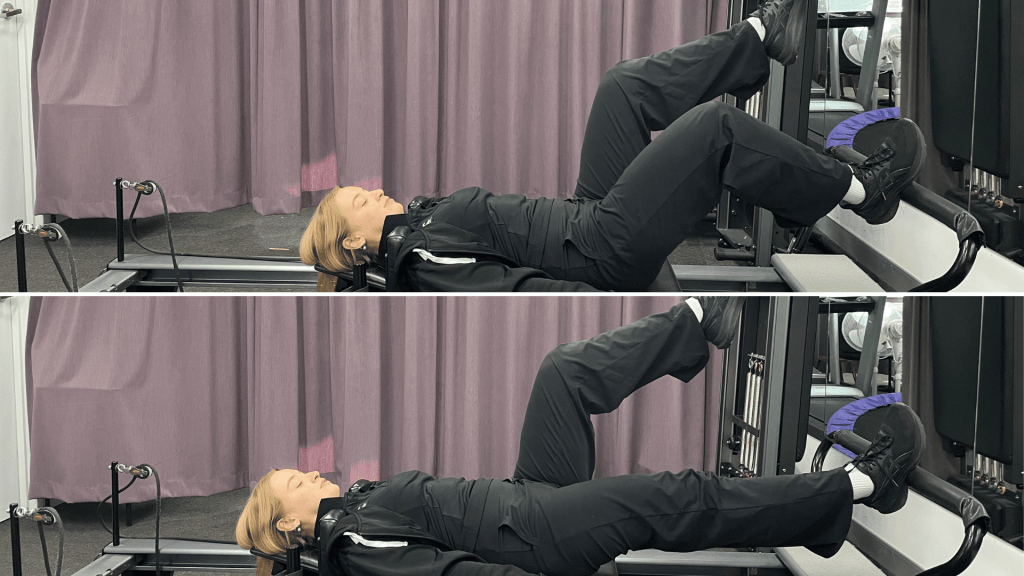
Aim: Improve gluteus Medius and core strength
How: Lay supine with one leg bent in “tabletop” position and one leg on the foot bar. With your core engaged push the carriage away and return slowly to the starting position. Ensure that your knee tracks in line with the second toe. Increase resistance by adjusting springs.
If you or someone you care for has an injury, a flare up, requires some rehabilitation or experiences an increase in pain, give the clinic a call on 9713 2455 or book online.